
Hospitals in East Sussex are overcrowded and experiencing ‘significant pressures’, councillors have heard.
The issue was raised at a meeting of the East Sussex Health Overview and Scrutiny Committee (HOSC) on Thursday (September 23), during a broader discussion of the county’s urgent care system.
Urgent care, as opposed to emergency care, is intended to provide treatment for pressing but non-life threatening health issues.
In recent years the NHS in East Sussex (and elsewhere) has been looking to strengthen this system through the introduction of NHS 111, weekend and evening GPs appointments and Urgent Treatment Centres (UTCs).
The intention behind the work is to prevent people going to A&E instead of using urgent care or same day primary care services (such as GPs).
But during discussion at HOSC, Hastings borough councillor Mike Turner (Lab) raised concerns about how well the system was functioning given recent pressures on the A&E department at Conquest Hospital.
He said:
“We are supposed to have more doctors in Hastings than the national average. When I asked the question why can’t anyone get appointments if that is the case I was told ‘we will get back to you on that’.
“At seven o’clock last night the A&E department at the Conquest Hospital was overwhelmed. There was nowhere even for people to sit, it was so bad. They were having to move to one side to allow people to even walk through the department.
“If we have got these GPs where are they? It seems to me to be a complete breakdown in the service.”
A similar point was raised by HOSC chairman Colin Belsey about pressures at the emergency department at Eastbourne DGH the previous weekend.
Joe Chadwick-Bell, chief executive of East Sussex Healthcare NHS Trust (ESHT), which runs both hospitals, gave more details about the situation.
She said:
“We have been experiencing really significant pressures, as I think we have discussed before.
“I think it is probably important to talk about the things we are trying to do. What we are trying to do is push more primary care presentations through our GPs and our emergency nurse practitioners.
“We are just working up an extended model and workforce model that would support us to be able to do that, because we have been struggling to get enough of that primary care type workforce to manage the level of demand.
“Secondly, we are absolutely overcrowded at the moment in terms of all of our wards. We have been up to 99 per cent occupancy.
“So what that means at the moment is we are struggling to get patients out of hospital and therefore if the beds are all full on the wards it is very difficult to move somebody out of A&E. Which means you get a lot of patients in A&E and therefore we don’t necessarily have space to see everyone in a timely way.”
Ms Chadwick-Bell went on to say there were action plans in place to reduce this pressure, both within the trust and on a wider local and countywide level. This was hoped to see improvements, she said.
She also said the trust’s A&E departments had generally been ‘good providers’ when measured against the four-hour wait standards, but had been experiencing issues over the last four to five weeks.
Following this, Geraldine Des Moulins, of the Voluntary Community and Social Enterprise (VCSE) Health and Wellbeing Alliance, asked what ‘blockages’ were causing the high occupancy on wards.
Ms Chadwick-Bell said the average length of stay was actually lower than it had been two years ago, i.e. people were leaving hospital sooner than in the past.
However, she said, the level of demand had increased at the same. In other words, more people were being admitted to hospital.
Even so, there were issues of patients being well enough to leave hospital but not able to move to a more appropriate place of care, Ms Chadwick-Bell added.
Following discussion HOSC asked for a further update on urgent care at a future meeting.

 Funding Available For Tree Planting In Chichester District as National Tree Week Begins
Funding Available For Tree Planting In Chichester District as National Tree Week Begins
 West Sussex Firefighters And Emergency Services Carry Out Training Exercise In Chichester Harbour
West Sussex Firefighters And Emergency Services Carry Out Training Exercise In Chichester Harbour
 Shoreham Lifeboat’s Festive Look Boosted By Family-Run Business
Shoreham Lifeboat’s Festive Look Boosted By Family-Run Business
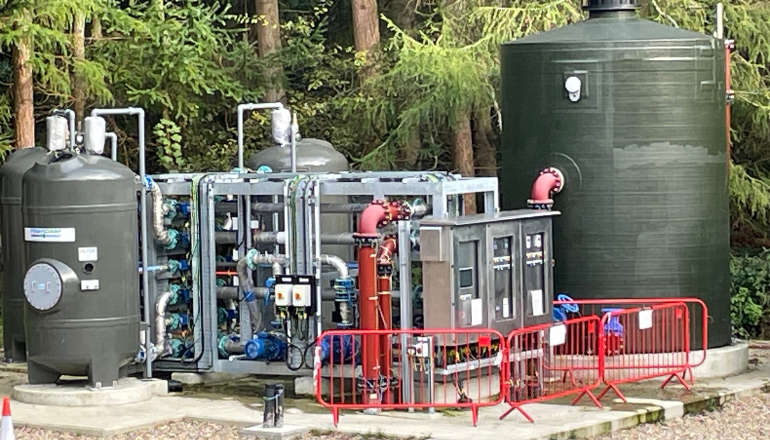 Final Touches Being Made To £2m Sussex Wastewater Site Upgrade
Final Touches Being Made To £2m Sussex Wastewater Site Upgrade
 AllSaints Founder To Host Sustainable Fashion Show In Brighton To Raise Money For Homelessness In City
AllSaints Founder To Host Sustainable Fashion Show In Brighton To Raise Money For Homelessness In City
 Chichester Community Warden Helping Fight Against Fraud This Christmas
Chichester Community Warden Helping Fight Against Fraud This Christmas
 Wealden Council Calls For Government Rethink On Winter Fuel Payment
Wealden Council Calls For Government Rethink On Winter Fuel Payment
 Snowy Protest At Lewes County Hall Calls For Fossil Fuel Divestment
Snowy Protest At Lewes County Hall Calls For Fossil Fuel Divestment
 Local MP Tours Firefighters’ Centre In Littlehampton
Local MP Tours Firefighters’ Centre In Littlehampton
 Former Portslade Scout Leader Convicted Of 79 Child Sex Offences
Former Portslade Scout Leader Convicted Of 79 Child Sex Offences